Report adverse events:
Adverse events should be reported to the Vifor Pharma group.
safety@viforpharma.com

I am practicing from:

Austria

Austria

Belgium

Germany

Ireland

Italy

Netherlands

Portugal

Spain

Switzerland
Other
I am residing in:

Austria

Austria

Belgium

Germany

Ireland

Italy

Netherlands

Portugal

Spain

Switzerland
Other

Bitte verwenden Sie als Benutzernamen die E-Mail Adresse, welche Sie bei der Registration angegeben hatten. Falls Sie das Passwort vergessen haben, können Sie sich einen Reaktivierungslink zustellen lassen. Alternativ ist für bereits registrierte Health Professionals auch eine Anmeldung mit der HPC-Card von FMH oder pharmaSuisse möglich.
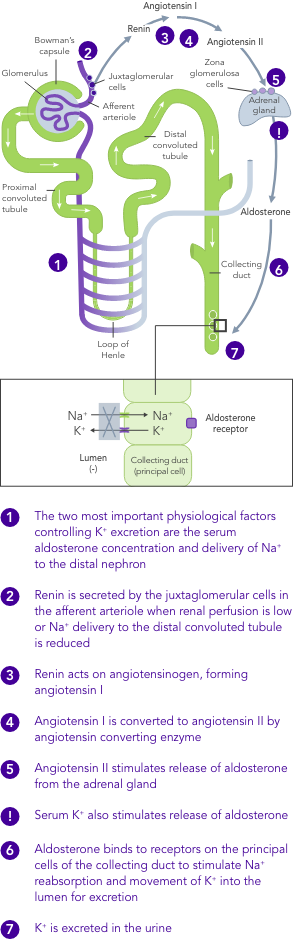
Hyperkalaemia, elevated serum K+ levels >5.0 mEq/L, is a serious condition associated with high morbidity and mortality1-6
Adverse events should be reported to the Vifor Pharma group.
safety@viforpharma.com
![]()
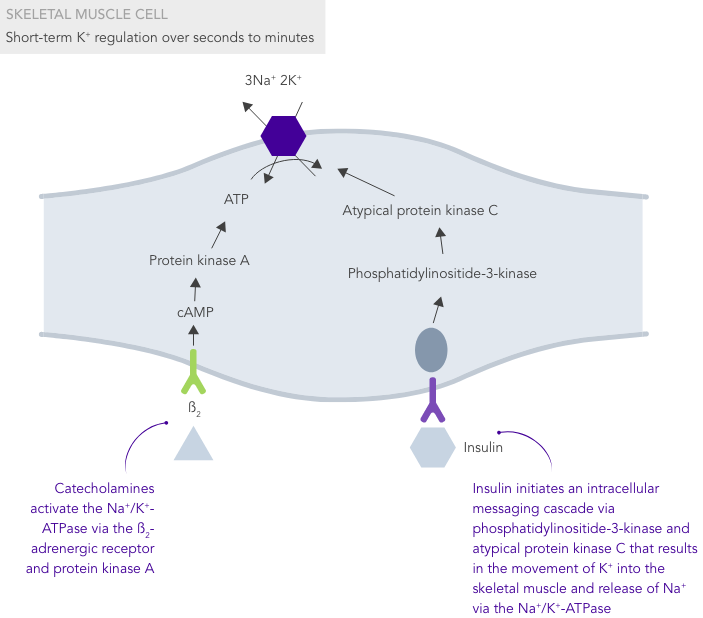
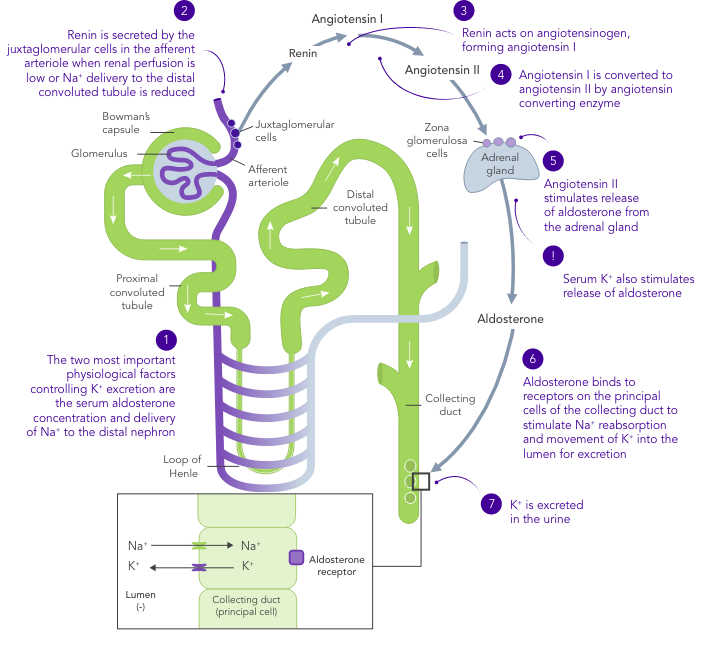
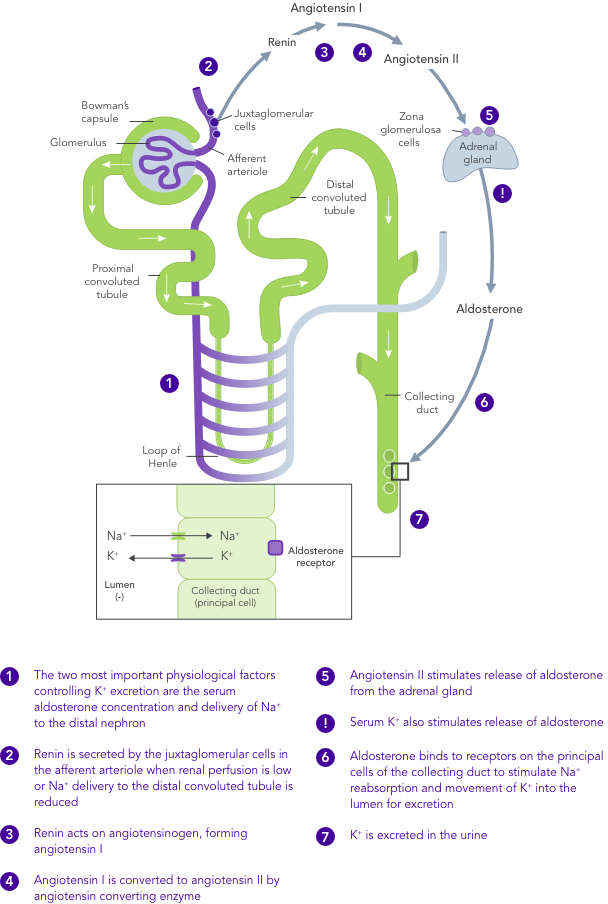
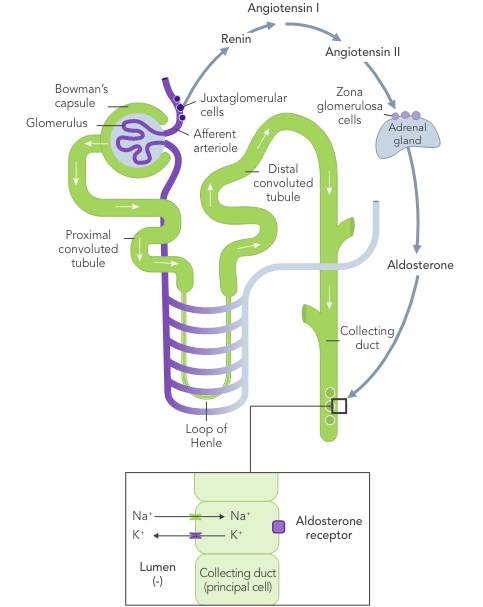
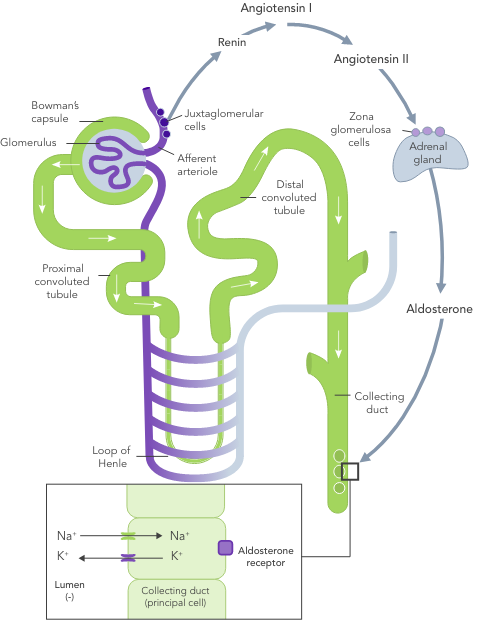
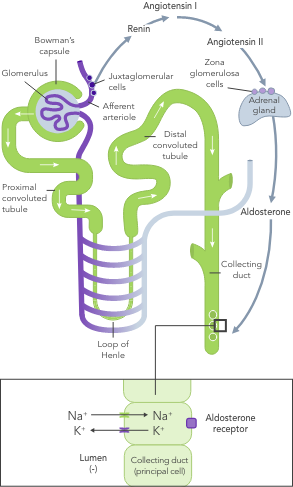
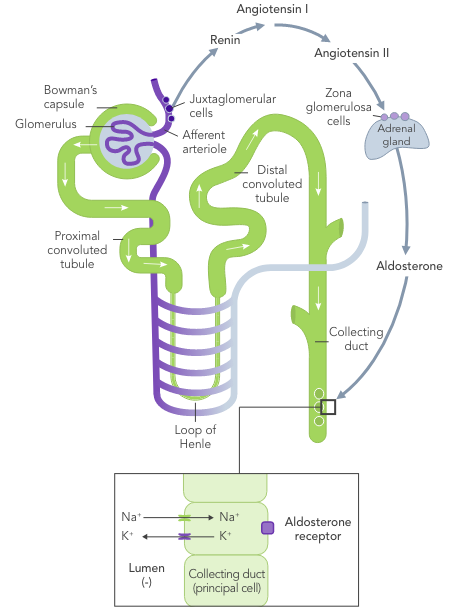
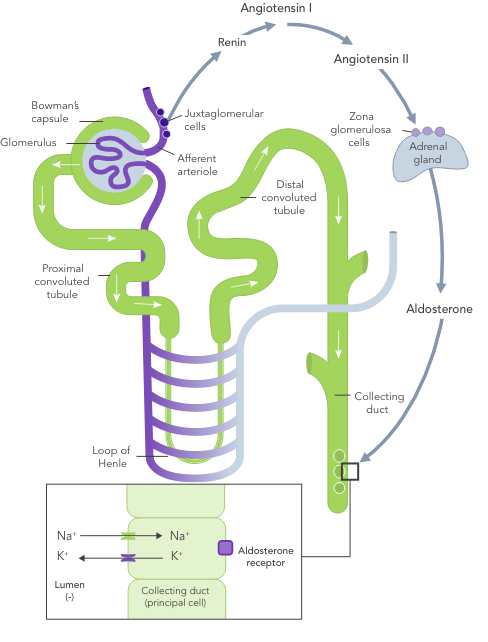
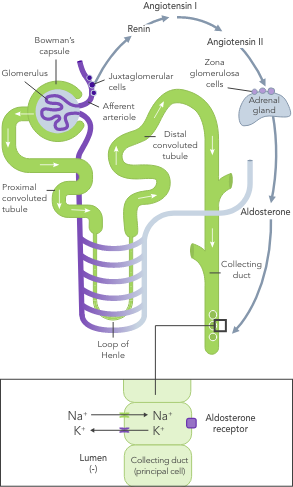
K+ homeostasis is achieved by long- and short-term control mechanisms.7,10
Chronic kidney disease
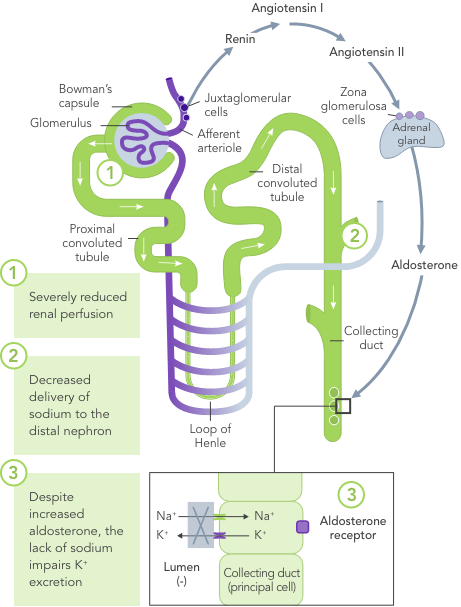
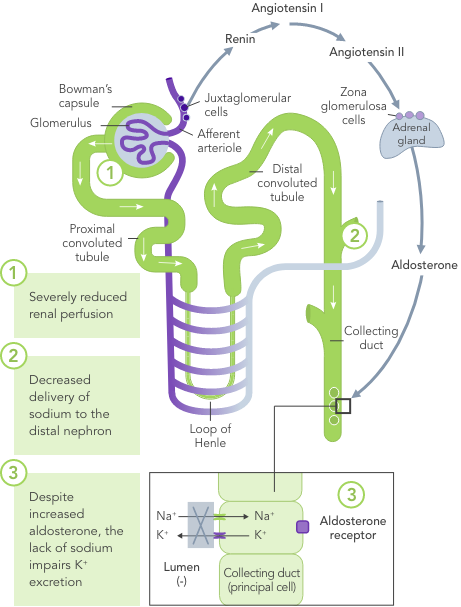
In CKD, K+ homeostasis, established mostly by excretion of K+ via urine, is deregulated and can result in hyperkalaemia
Heart failure
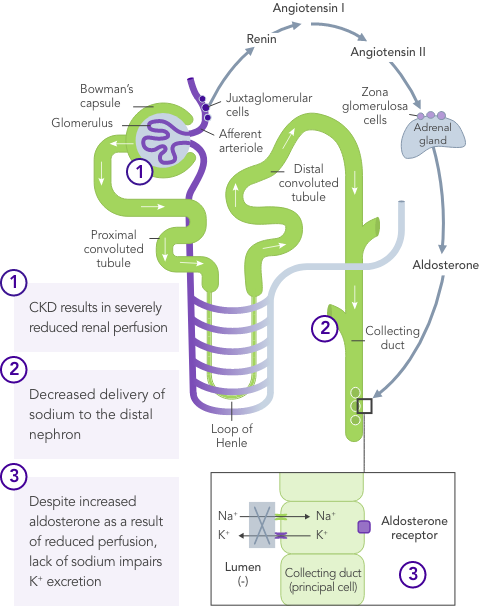
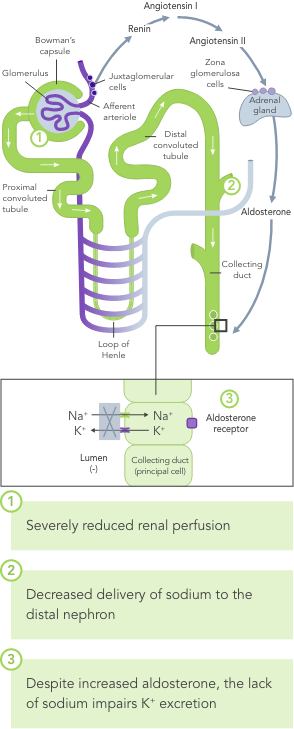
In HF, the RAAS is up-regulated, renal perfusion is reduced and Na+ is often excreted due to usage of diuretics
Diabetes mellitus
Due to the lack of insulin-stimulated Na+/K+ pump-mediated K+ uptake in skeletal muscles
Age
Age-dependent reduction in the availability of nephrons further increases the risk for hyperkalaemia
Medication
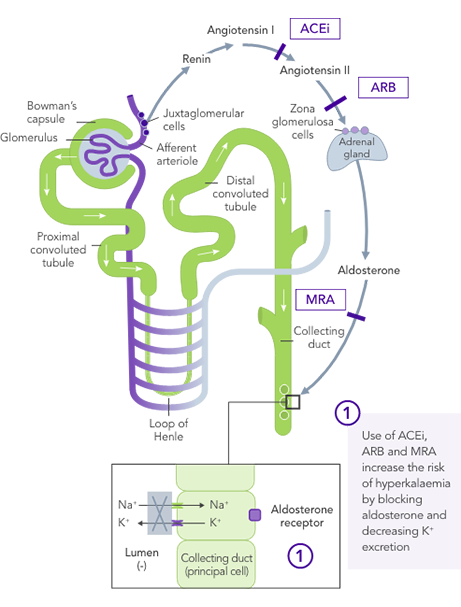
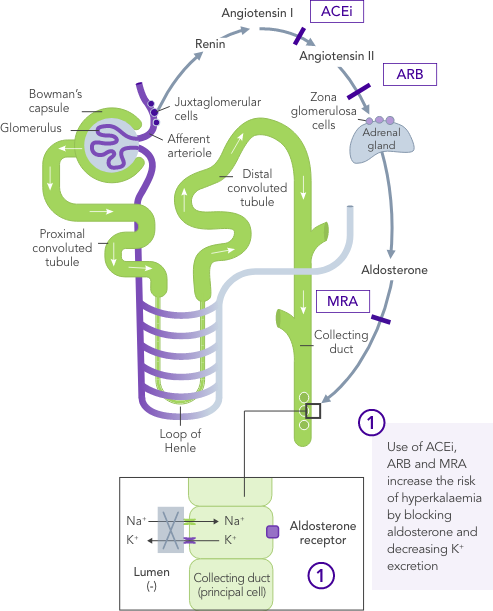
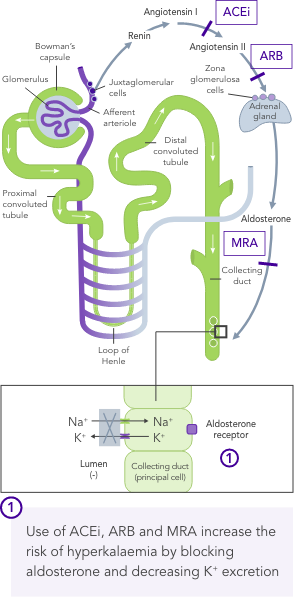
Background use of RAASi, beta blockers and aldosterone antagonists are associated with an increase in K+ levels
Exercise
Because skeletal muscles constitute the major reservoir for K+ in the body, K+ levels may increase markedly and reach values up to ~8 mEq/L during exercise
Intake of K+
Oral K+ intake combined with reduced K+ excretion can increase risk of hyperkalaemia
Hyperkalaemia is one of the most clinically important electrolyte abnormalities and is a serious medical condition associated with increased mortality and high rates of hospitalisation.1,3,4,6
In a targeted retrospective chart review of 1,457 patients with hyperkalaemia in 5 centres in Europe, hyperkalaemia was responsible for over one-third of hospitalisations over a 12-month period.6

36%
Hyperkalaemia
related
![]()
1,457
Patients
![]()
72%
With HTN
![]()
68%
With CKD
![]()
40%
With HF
![]()
36%
With T2DM
![]()
60.5%
With RAASi
The effects of hyperkalaemia can vary widely between patients,15 with symptoms ranging from mild and non-specific (e.g. muscle weakness, twitching, cramping, nausea, vomiting) to arrhythmias, palpitations, dizziness and syncope, and sudden cardiac death.3,16
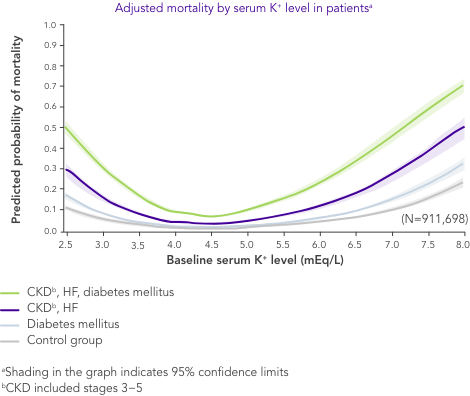
Although severity of clinical presentation generally correlates with degree of hyperkalaemia,2 physiological adaptation, structural cardiac disease, medication use, and degree of concurrent illness might predispose certain patients with hyperkalaemia to a lower or higher threshold for toxicity.17

Importantly, hyperkalaemia is often asymptomatic until the patient experiences serious consequences.2,16 ECG changes are not always present but can progress rapidly without warning, making hyperkalaemia with ECG changes a true medical emergency.2
CKD is the most common risk factor for hyperkalaemia.
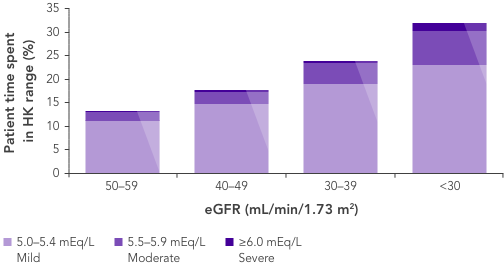
In patients with CKD, the ability to maintain K+ homeostasis is compromised as a result of reduced GFR, leading to an increased risk of hyperkalaemia.






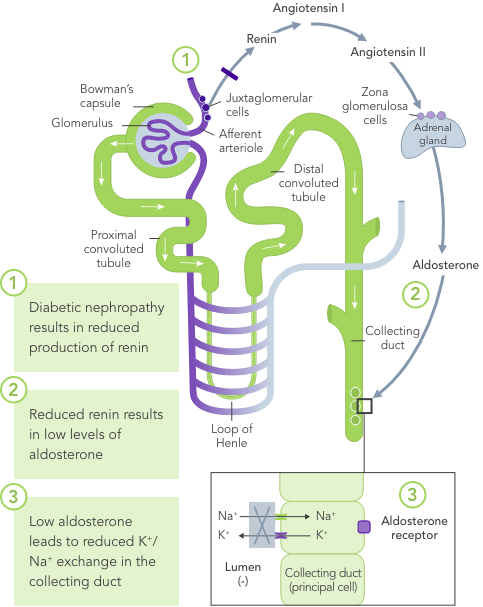
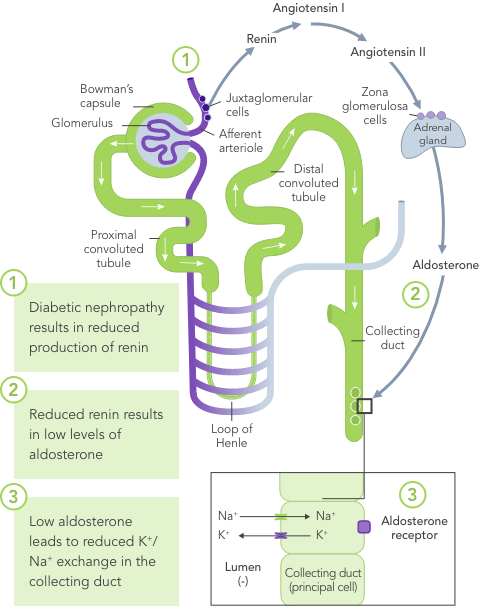
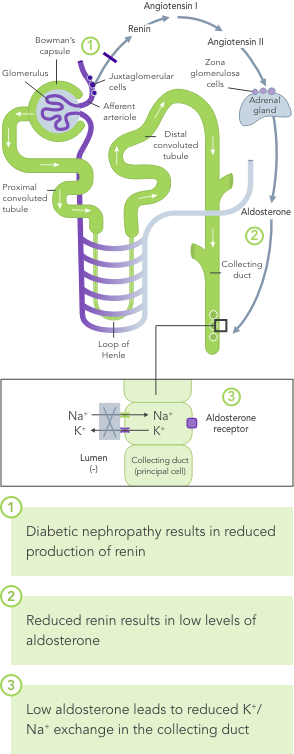

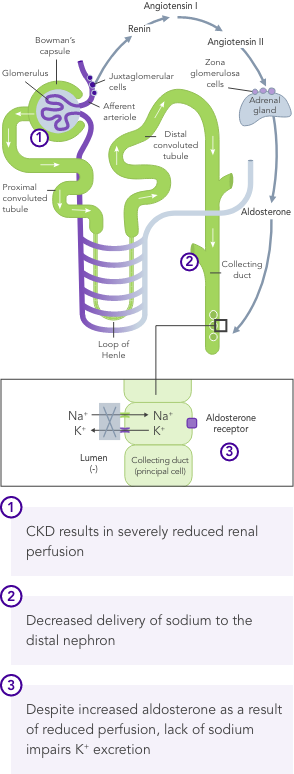
Chronic hyperkalaemia requires ongoing management to correct the underlying disturbances in K+ balance.21
Onset of hyperkalaemia symptoms can be sudden22 and require urgent treatment.
Hyperkalaemia often leads to RAASi down-titration or discontinuation, and this is associated with poor outcomes in patients with CKD.25,26
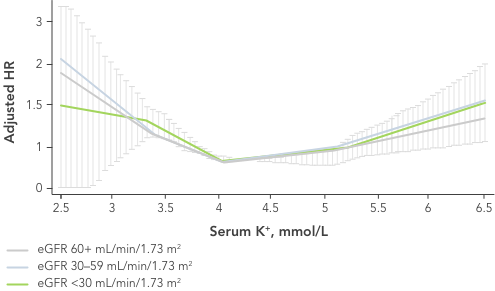
Almost 4 in 10 patients with HF develop hyperkalaemia27,28 and many have recurrent episodes, with time between episodes becoming progressively shorter.27
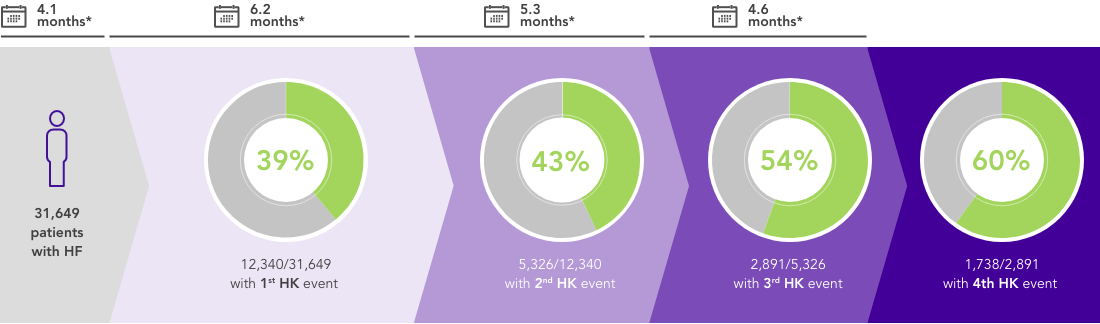
*Median follow-up
Patients with HF are at risk of hyperkalaemia as approximately one-third to one-half have impaired renal function (eGFR <60 mL/min/1.73 m2).29






Even a small increase in K+ levels may increase risk of mortality.4
Onset of hyperkalaemia symptoms can be sudden22 and require urgent treatment.
Hyperkalaemia is a risk marker for poor outcomes in patients with HF through suboptimal use of RAASi.25,31,32
ACEi, angiotensin II converting enzyme inhibitor; ARB, angiotensin II-receptor blocker; cAMP, cyclic adenosine monophosphate; CI, confidence interval; CKD, chronic kidney disease; ECG, electrocardiogram; (e)GFR, (estimated) glomerular filtration rate; HF, heart failure; HK, hyperkalaemia; HTN, hypertension; K+, potassium ions; mEq/L, milliequivalents per litre; MRA, mineralocorticoid-receptor antagonist; Na+, sodium ions; RAASi, renin−angiotensin−aldosterone system inhibitors; T2DM, type 2 diabetes mellitus.
1. Di Lullo L, et al. Cardiorenal Med 2019;9(1):8−21. 2. Rastegar A, Soleimani M. Postgrad Med J 2001;77(914):759−64. 3. Kjeldsen KP, Schmidt TA. Eur Heart J 2019;21(Suppl A):A2−A5. 4. Collins AJ, et al. Am J Nephrol 2017;46(3):213−21. 5. Kovesdy CP, et al. Eur Heart J 2018;39(17):1535−42. 6. Rossignol P, et al. Clin Kidney J 2020;13:714−9. 7. Clase CM, et al. Kidney Int 2020;97(1):42−61. 8. Youn JH, McDonough AA. Annu Rev Physiol 2009;71:381−401. 9. Palmer BF. Clin J Am Soc Nephrol 2015;10(6):1050−60. 10. Palmer BF. N Engl J Med 2004;351:585−92. 11. Mathialahan T, et al. J Pathol 2005;206:46−51. 12. Rosano GMC, et al. Eur Heart J Cardiovasc Pharmacother 2018;4(3):180−8. 13. Tromp J, van der Meer P. Eur Heart J 2019;21(Suppl A):A6−A11. 14. Palmer BF. In: Kimmel PL, Rosenberg M (Eds). 2015:386−7. 15. Welch A, et al. Nephrol Dial Transplant 2013;28(1):15−16. 16. Kraft MD, et al. Am J Health Syst Pharm 2005;62(16):1663−82. 17. Montford JR, Linas S. J Am Soc Nephrol 2017;28(11):3155−65. 18. Kashihara N, et al. Kidney Int Rep 2019;4(9):1248−60. 19. Einhorn LM, et al. Arch Intern Med 2009;169(12):1156−62. 20. Luo J, et al. Clin J Am Soc Nephrol 2016;11(1):90−100. 21. Kim GH. Electrolyte Blood Press 2019;17(1):1−6. 22. Dasgupta A. E-Journal of Cardiology Practice 2016;14, No 13. https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-14/fourteen-thirteen. 23. Betts KA, et al. Kidney Int Rep 2018;3(2):385−93. 24. Provenzano M, et al. J Clin Med 2018;7:499. DOI:10.3390/jcm7120499. 25. Epstein M, et al. Am J Manag Care 2015;21(11 Suppl):S212−S220. 26. Yildirim T, et al. Ren Fail 2012;34(9):1095−9. 27. Thomsen RW, et al. J Am Heart Assoc 2018;7(11):e008912. 28. Savarese G, et al. JACC Heart Fail 2019;7(1):65−76. 29. Shlipak MG. Ann Intern Med 2003;138(11):917−24. 30. Núñez J, et al. Circulation 2018;137:1320–30. 31. Lund LH, Pitt B. Eur J Heart Fail 2018;20:931–2. 32. Martens P, et al. Acta Cardiol 2020; doi: 10.1080/00015385.2020.1771885.