Hyperkalaemia is a highly prevalent condition in your patients with chronic kidney disease1 and can jeopardise their beneficial RAASi therapy2,3
Help us guide you to the right place
I reside in the United States
Visit the US site
Help us guide you to the right place
I am practicing from:

Austria
-

Austria
-

Belgium
-

Germany
-

Ireland
-

Italy
-

Netherlands
-

Portugal
-

Spain
-

Switzerland
-
Other
Help us guide you to the right place
I am residing in:

Austria
-

Austria
-

Belgium
-

Germany
-

Ireland
-

Italy
-

Netherlands
-

Portugal
-

Spain
-

Switzerland
-
Other

Bitte verwenden Sie als Benutzernamen die E-Mail Adresse, welche Sie bei der Registration angegeben hatten. Falls Sie das Passwort vergessen haben, können Sie sich einen Reaktivierungslink zustellen lassen. Alternativ ist für bereits registrierte Health Professionals auch eine Anmeldung mit der HPC-Card von FMH oder pharmaSuisse möglich.
please proceed.
HYPERKALAEMIA challenge in CKD
Report adverse events:
Adverse events should be reported to the Vifor Pharma group.
safety@viforpharma.com
RAASi therapy is vital
Progression of CKD to kidney failure, the avoidance or delay in initiating dialysis therapy, and the risks associated with dialysis are critically important to patients.4
- RAASi have been shown to slow kidney function decline more effectively than other blood pressure-lowering drugs and to reduce proteinuria.4-6
RAASi are the cornerstone of therapy in CKD, and their use at the highest tolerated dose is recommended by multiple organisations4,7
- Two landmark trials (IDNT8: Irbesartan Diabetic Nephropathy Trial and RENAAL9: Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist Losartan) were conducted in patients with T2DM and CKD with albuminuria >1 g/d.
- The renoprotective effect of these drugs was evidenced by a
16–20% reduction in the composite endpoint of risk of death, progression to dialysis or doubling for serum creatinine.4,8,9 - Ramipril use in patients with non-diabetic nephropathy has also been shown to have a renoprotective effect, reducing both proteinuria and the rate of GFR decline.10
IDNT and RENAAL: reduced risk of death, ESRD, or doubling of serum creatinine concentration with RAASi8,9
IDNT8
Patient population:
1,715
Patients with diabetic nephropathy
Treatment:
Once daily irbesartan 300 mg, amlodipine 10 mg or placebo
Primary endpoint:
Composite of death, ESRD or doubling of
baseline serum creatinine
Mean follow-up:
2.6
years
Risk reduction in primary endpoint:
20%
vs placebo
(p=0.02)
23%
vs amlodipine
(p=0.006)
RENAAL9
Patient population:
1,513
Patients with diabetic nephropathy
Treatment:
Once daily losartan 50−100 mg or placebo
Primary endpoint:
Composite of death, ESRD or doubling of
baseline serum creatinine
Mean follow-up:
3.4
years
Risk reduction in primary endpoint:
16%
vs placebo
(p=0.02)
HYPERKALAEMIA risk is exacerbated by RAASi
Guideline-directed use of RAASi has been cited as a major factor in the development of hyperkalaemia in patients with CKD.11
- In clinical trials, RAASi have been shown to increase the risk of hyperkalaemia in patients with CKD.12
- Real-world studies consistently show an approximate 1.5-fold increased risk of hyperkalaemia in patients on RAASi,13,14 with risk increasing with severity of kidney disease.15
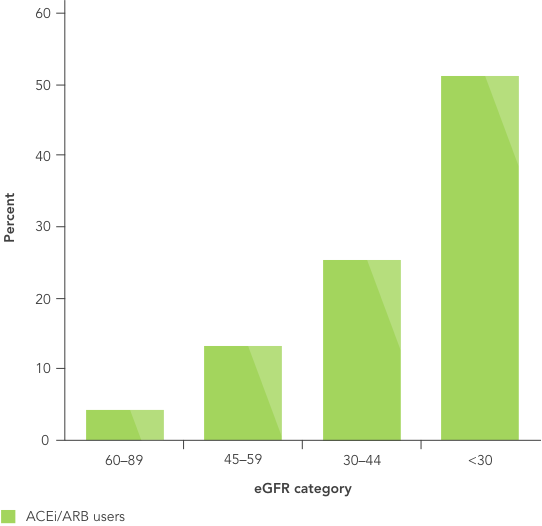
Proportion of patients with hyperkalaemia during the first year of therapy with RAASi increases with severity of kidney disease15
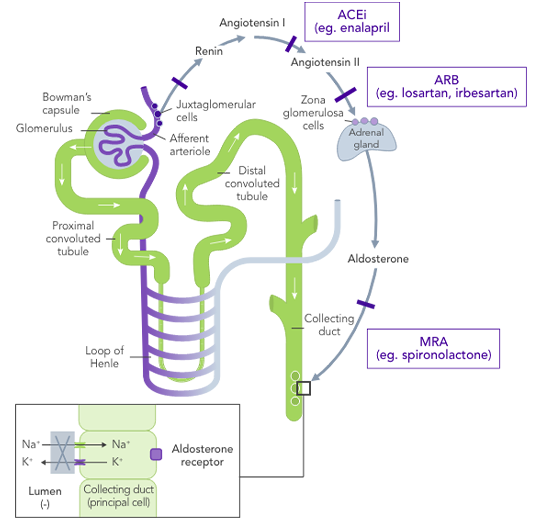
The impact of RAASi on the renin−angiotensin−aldosterone system
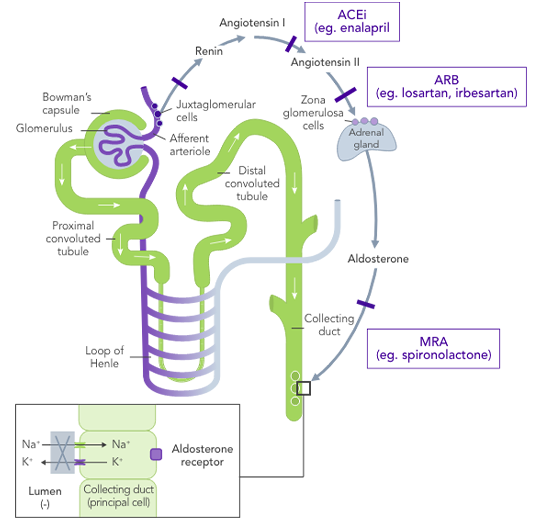
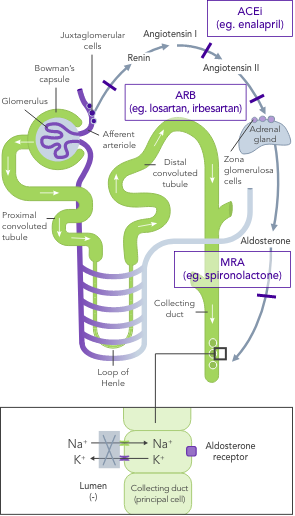
hyperkalaemia


angiotensin−aldosterone system


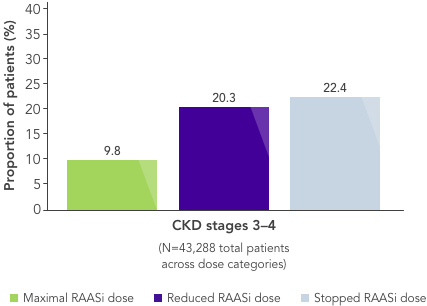
HYPERKALAEMIA leads to suboptimal RAASi use
Current guidelines recommend dose reduction or discontinuation of RAASi if persistent hyperkalaemia is a problem in patients with CKD. As a result, hyperkalaemia is one of the main reasons for withholding RAASi treatment.2,3
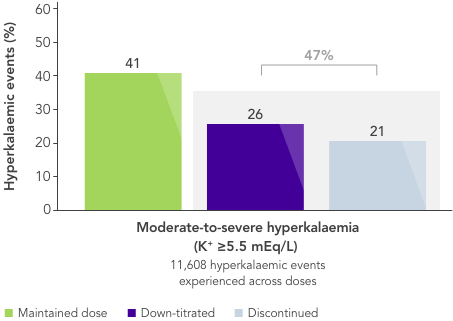
- In a large US database analysis,2 ~40% and ~50% of patients on maximum RAASi dose experiencing mild or moderate-to-severe hyperkalaemia, respectively, had their dose reduced or stopped after a hyperkalaemic event.
Nearly half of patients on maximal RAASi dose have their treatment reduced or stopped after a hyperkalaemia event2
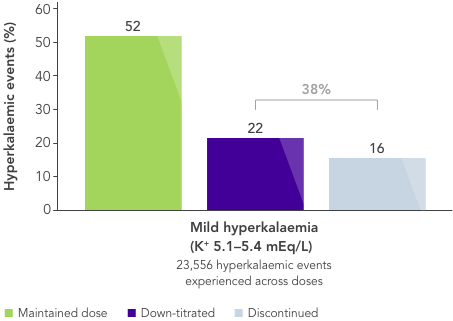
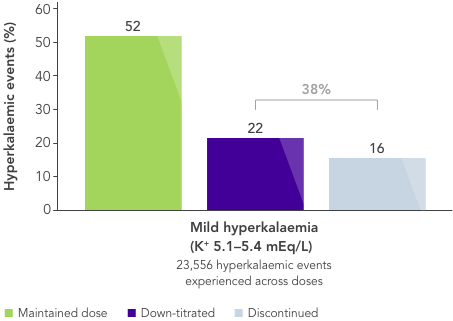
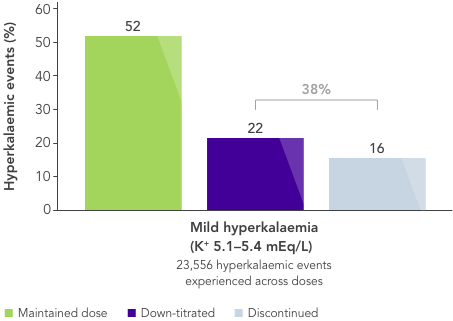
Nearly half of patients on maximal RAASi dose have their treatment reduced or stopped after a hyperkalaemia event2
hyperkalaemia


hyperkalaemia


However, reducing or stopping RAASi is associated with an increased risk of mortality and morbidity.2,16
![]()
Physicians, therefore, are often faced with the dilemma of using RAASi and accepting hyperkalaemia or reducing/stopping RAASi and accepting poorer clinical outcomes
What is needed is a therapy that allows CKD patients to stay on beneficial RAASi therapy with reliable long-term control of serum K+ levels.
Mortality risk doubles when RAASi is reduced or stopped2
Current treatment options for chronic HYPERKALAEMIA are limited
Both short- and long-term treatment strategies are critical for the management of hyperkalaemia.17 However, currently available options focus mainly on emergency and intermediate care,17 and there are substantial limitations associated with current treatment options for chronic hyperkalaemia:
Dietary modifications may lead to restricted consumption of healthy foods,18 and it may be very difficult for patients already on a restricted diet to adhere to further dietary modifications.19,20 The effects of dietary interventions on outcomes are uncertain.19
Non-K+-sparing loop diuretics depend on residual renal function and are associated with increased risk of gout and diabetes, volume contraction and reduced potassium excretion, and sarcopenia.17,21
Traditional K+-binders (SPS and CPS) can be associated with life-threatening GI side effects and hypokalaemia22,23 and may not be suitable in those who cannot tolerate an increase in sodium (SPS).23

There is an unmet need for a reliable long-term option for the management of chronic hyperkalaemia that enables patients to continue RAASi therapy at target doses.17
ACEi, angiotensin II converting enzyme inhibitor; ARB, angiotensin II-receptor blocker; CKD, chronic kidney disease; CPS, calcium polystyrene sulfonate; ESRD, end-stage renal disease; eGFR, estimated glomerular filtration rate; GI, gastrointestinal; HK, hyperkalaemia; IDNT, Irbesartan Diabetic Nephropathy Trial; K+, potassium ions; MRA, mineralocorticoid-receptor antagonist; Na+, sodium ions; NIDDM, non-insulin-dependent diabetes mellitus; RENAAL, Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist Losartan; RAASi, renin−angiotensin−aldosterone system inhibitors; RR, relative risk; SPS, sodium polystyrene sulfonate; T2DM, type 2 diabetes mellitus; US, United States.
References:
1. Rosano GMC, et al. Eur Heart J Cardiovasc Pharmacother 2018;4(3):180−8. 2. Epstein M, et al. Am J Manag Care 2015;21(11 Suppl):S212−S220. 3. Yildirim T, et al. Ren Fail 2012;34(9):1095−9. 4. KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int 2020;98(Suppl 4S):S1–S116. 5. KDIGO Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl 2013;3:1–150. 6. National Kidney Foundation. K/DOQI Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease. 2004. Available at: kidneyfoundation.cachefly.net/professionals/KDOQI/guidelines_bp/index.htm (accessed July 2020). 7. National Institute for Health and Care Excellence. Chronic kidney disease in adults: assessment and management. 2014. Available at: http://www.nice.org.uk/CG182 (accessed April 2020). 8. Lewis EJ, et al. N Engl J Med 2001;345(12):851−60. 9. Brenner BM, et al. N Engl J Med 2001;345(12):861−9. 10. The GISEN Group. Lancet 1997;28;349(9069):1857−63. 11. Palmer BF. N Engl J Med 2004;351(6):585−92. 12. Georgianos PI, Agarwal R. Kidney Int 2018;93(2):325−34. 13. Nilsson E, et al. Int J Cardiol 2017;245:277−84. 14. Einhorn LM, et al. Arch Intern Med 2009;169(12):1156−62. 15. Bandak G, et al. J Am Heart Assoc 2017;6(7):e005428. 16. Qiao Y, et al. JAMA Intern Med 2020;180(5):718−26. 17. Dunn JD, et al. Am J Manag Care. 2015;21(15 Suppl):S307−S315. 18. National Kidney Foundation. The DASH Diet. Available at: kidney.org/atoz/content/Dash_Diet (accessed July 2020). 19. Palmer SC, et al. Cochrane Database Syst Rev 2017;4:CD011998. 20. Vendramini LC, et al. Braz J Med Biol Res 2012;45(9):834−40. 21. Ishikawa S, et al. PLOS One 2018;13:1–16. 22. Calcium Resonium PI. Sanofi 2018. 23. Kayexalate® US PI. Sanofi 2017.



